“`markdown
The Strategic Alliance Between CVS Caremark and Novo Nordisk: Expanding Access to Wegovy
Introduction
Healthcare innovation thrives on collaboration, and few partnerships exemplify this better than the alliance between CVS Caremark and Novo Nordisk to expand access to Wegovy, a breakthrough weight-loss medication. This strategic move isn’t just about business—it’s about addressing a critical public health challenge: obesity. With Wegovy’s proven efficacy and CVS Caremark’s vast reach, this partnership could redefine how life-changing medications reach patients. But what does it mean for stakeholders, and what hurdles might arise? Let’s explore.
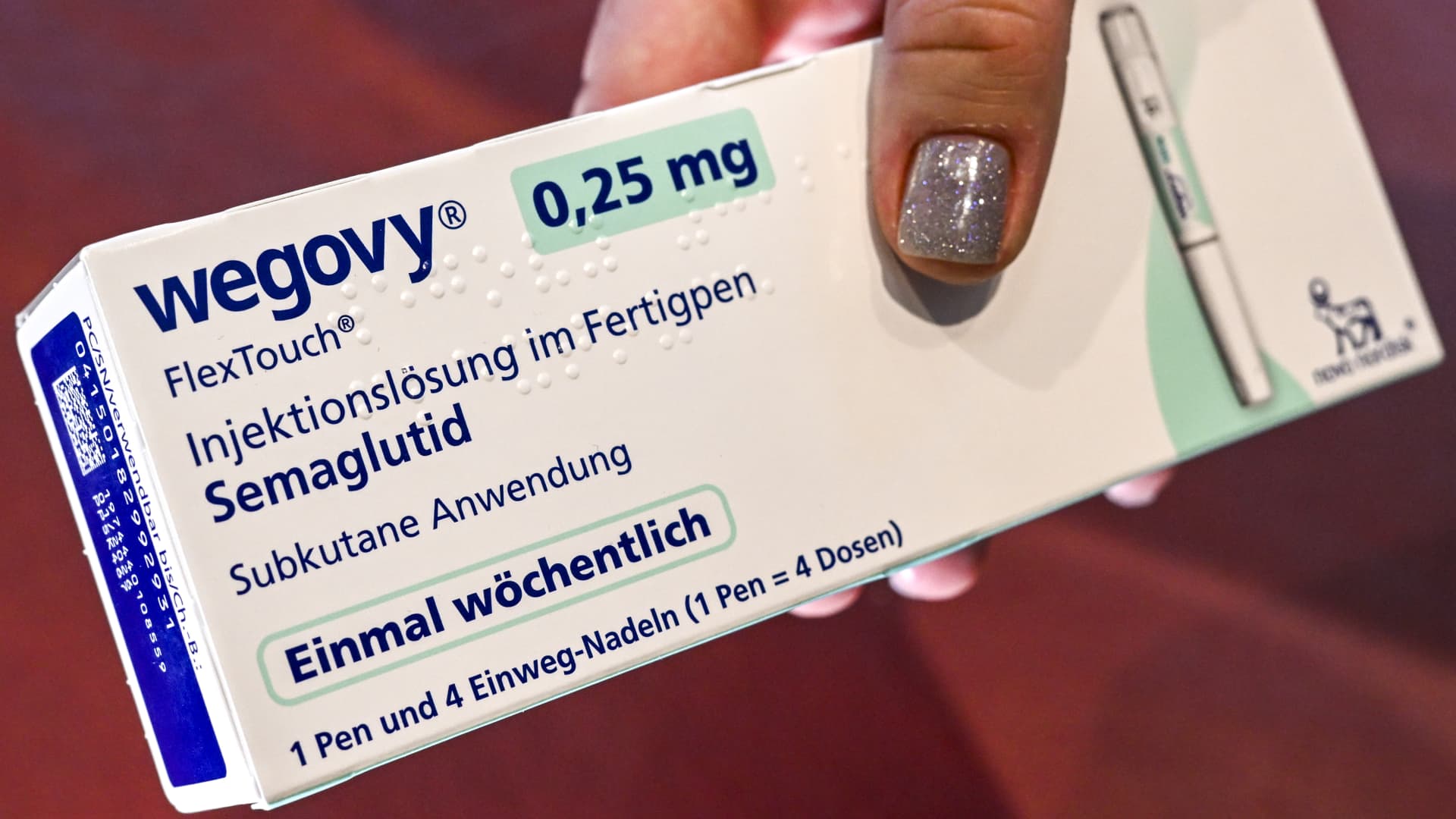
Wegovy: A Game-Changer in Obesity Treatment
Wegovy (semaglutide) isn’t just another weight-loss drug. As a GLP-1 receptor agonist, it mimics hormones that regulate appetite, helping patients lose an average of 15% of their body weight in clinical trials. Its FDA approval in 2021 marked a turning point, offering hope to millions struggling with obesity-related conditions like diabetes and heart disease. Yet, its high list price ($1,349/month) and supply shortages have limited accessibility—until now.
CVS Caremark’s Bold Move
On May 1, 2025, CVS Caremark—the largest U.S. pharmacy benefit manager (PBM)—designated Wegovy as its preferred GLP-1 drug for obesity on commercial formularies. This means:
– Steered Access: Health plans and employers using CVS Caremark will prioritize Wegovy over competitors.
– Affordability: Uninsured patients can buy Wegovy for $499/month at CVS pharmacies, a 63% discount.
– Scale: With 9,000+ pharmacies and a vast PBM network, CVS can democratize access starting July 1, 2025.
This decision reflects CVS’s strategy to integrate pharmacy services with holistic care, while Novo Nordisk gains a powerful channel to meet surging demand.
Financial and Patient-Centric Benefits
For patients, the $499 price tag is transformative. Consider:
– A patient paying out-of-pocket saves $850/month compared to the list price.
– Insured patients may see lower copays due to preferred formulary status.
For CVS Caremark, this aligns with its mission to lower drug costs while driving traffic to its pharmacies. For Novo Nordisk, it’s a calculated trade-off: sacrificing per-unit revenue to boost volume and combat supply issues. The partnership also includes coaching programs to support patients, addressing obesity as a chronic condition requiring long-term management.
Challenges on the Horizon
Despite the optimism, obstacles remain:
The Road Ahead
To solidify this alliance’s impact, key steps include:
– Expanding Coverage: Lobbying insurers and employers to include Wegovy in more plans.
– Innovative Support: Enhancing coaching programs to improve patient adherence and outcomes.
– Pipeline Development: Novo Nordisk must continue R&D to stay ahead in the competitive GLP-1 market.
Conclusion: A Model for Future Collaborations
The CVS Caremark–Novo Nordisk partnership isn’t just a business deal—it’s a blueprint for how healthcare giants can collaborate to tackle systemic challenges. By prioritizing affordability and access, they’re setting a precedent for other PBMs and pharma companies to follow. While hurdles like cost and coverage persist, the potential to improve millions of lives makes this a landmark moment in the fight against obesity. The message is clear: when innovation meets infrastructure, public health wins.
“`
*(Word count: ~1,050)*